Eye Surgeon Ophthalmologist
What is Refractive Surgery?
Refractive Surgery is surgery on the Eye that corrects refractive errors, such as myopia, hyperopia, astigmatism and often presbyopia.
There is now an experience of about 30 years in the Ophthalmological community now with the very advanced laser machines, which allow us to have predictable, exceptional and accurate results.
To achieve clear vision, the cornea and lens must refract light rays appropriately to focus the image on the retina.

The cornea is responsible for about 2/3 of the total, usually 60 diopters of optical refractive power. Unlike the lens, which can change its refractive power through adjustment, the corneal curvature is constant. The cornea consists of 5 layers that provide a transparent tissue and refractive power to the eye. Laser vision correction removes stratum corneum of the cornea to change its shape, making it flatter or curved.
The goal of laser correction is to get rid of glasses and contact lenses.
What are the mandatory criteria for someone to undergo Laser surgery to correct refractive errors?

It must first be examined by an ophthalmologist and depending on the case, the history and the reasons he wishes, the doctor will decide if he can safely undergo such an operation.
It is obligatory for him to have completed the 18th year of age, and the refraction (his glasses) to be stable for at least one year. If there is no serious reason for haste, we can delay the operation a little until 20-21 years, when the development of the body is completed and therefore a small possible increase in myopia.
a) Who can have laser myopia safely?
People with myopia up to 10 degrees, as well as people with hyperopia or astigmatism up to 5-6 degrees who do not want to wear glasses for aesthetic reasons or have problems with their contact lenses (intolerance to contact lenses). Those who can not easily wear glasses at work, athletes or those who do intense sports.
Who Cannot Have a Laser (Contraindications)
It is contraindicated for those who have ophthalmic diseases such as keratoconus (clinical or subclinical) or other extensive corneal diseases, severe dry eye, very thin cornea, active corneal infection, growing muscle.
Related contraindications are a history of herpetic keratitis, previous eye surgery, corneal scarring, diabetes mellitus, autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus), risk of developing glaucoma and other specific glaucoma. There is a contraindication to pregnant women and breastfeeding.
How is laser correction done? What are the techniques?
Refractive surgery is performed using the excimer laser that sculpts the cornea to modify its curvature. The rays of light then focus on the retina (the back of the eye) so that the image of the object we see is clearly formed (ie we can see it clearly). There are two main techniques:
PRK: Photorefractive keratectomy

In PRK access to the stratum corneum is achieved by removing the epithelium mechanically (e.g. by swirling) or chemically (with alcohol). The patient then focuses on a central light. A mechanism
eye tracker is engaged to adapt to any eye movement and a predetermined excision (photo-removal) of the cornea is performed, within a few seconds, proportional to the pre-existing refraction (degrees of refractive error) with the eximer. Intraoperative deposition of a specific drug minimizes the possibility of postoperative haze. Finally, a therapeutic contact lens is placed that remains until the epithelium is completely healed (a few days).
Recently access to the mattress has been achieved with the laser itself.
This method is called Trans-PRK Photorefractive keratectomy and is now ideal, since the whole procedure is achieved without any eye contact with the surgeon (no touch laser).
Thus, laser vision correction with excimer laser is an increasingly popular and safe procedure that has provided ideal vision to patients around the world.
The operation is performed with anesthetic drops and is very safe, more so than the use of contact lenses. The application of the laser takes less than a minute, while the whole procedure takes no more than 8-10 minutes for both eyes. The patient leaves the operating room without bandages and without the need for glasses.
LASIK: Laser in situ corneal extraction (laser in situ)
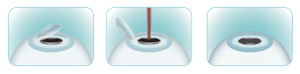 The surgeon creates a flap (flap 100-160μm) in the cornea using an infrared femtosecond laser, as now the mechanical keratome is rarely used. The surgeon then lifts the flap and follows the excimer laser that sculpts the corneal layer. The surgeon then restores the flap to its original position and the operation ends. The operation is completely painless, only with anesthetic drops. The application of the laser lasts less than 1 minute in each eye.No sutures, no postoperative pain. The whole procedure in the operating room is about 10-15 minutes for both eyes.
The surgeon creates a flap (flap 100-160μm) in the cornea using an infrared femtosecond laser, as now the mechanical keratome is rarely used. The surgeon then lifts the flap and follows the excimer laser that sculpts the corneal layer. The surgeon then restores the flap to its original position and the operation ends. The operation is completely painless, only with anesthetic drops. The application of the laser lasts less than 1 minute in each eye.No sutures, no postoperative pain. The whole procedure in the operating room is about 10-15 minutes for both eyes.
After all, which technique is the best?
 If the eye is “good” (receptive), with a thick cornea, good preoperative examinations are often possible for both techniques. The result is just as good in the month with both techniques.
If the eye is “good” (receptive), with a thick cornea, good preoperative examinations are often possible for both techniques. The result is just as good in the month with both techniques.
The surgeon finally chooses the technique, depending on the needs of the individual and mainly based on the parameters of his eye in detail, always guided by the safety of the patient.
The fempto-LASIK technique has very fast restoration of vision and zero discomfort after surgery. But it is a more “invasive” technique than PRK. PRK is a relatively safe laser surgery, and especially in Trans-PRK a “no touch” laser is applied. Dry eye as a complication is statistically smaller. The disadvantage, however, is that the restoration of vision is more gradual, there are postoperative discomforts for a few days and it requires more postoperative visits.
What are preoperative examinations?
The examination by the Ophthalmologist who will operate on you is very basic. Accurate correct refraction (measurements) is a very important part of the whole process. There will be careful examination of the slit lamp, keratometry, refractive examination with precision, eclipse, measurement of the maximum corrected visual acuity, examination of the “dominant” eye, pressure control, corneal dry eye examination, coronary artery disease, lesions, etc.
Depending on the age, a corresponding target will be made for the final desired result in each eye.
The candidate must not wear contact lenses 14 days before the surgery. He will undergo special painless corneal examinations (corneal tomography (pentagam)) corneal topography (orbscan) and other examinations to rule out keratoconus or other parameters of possible destabilization with ocular surgery. PRK surgery The final choice is always discussed with the candidate and is chosen by the Ophthalmologist Surgeon.
What the postoperative instructions include
Do not rub your eyes and do not get tap water for the next 10-15 days.
Avoid makeup, swimming for 20 days. Beware of dust and smoky areas.
Eye drops: antibiotics, cortisone and artificial tears.
Use covers that are given to you so that you do not rub your eyes in sleep. On the day of the operation, keep your eyes closed. Avoid TV, reading, computer.
If you have done LASIK you will not have pain, your quantitative vision the next day will be very good, your quality vision will take days. If you have done trans-PRK or PRK, the discomfort will last for 2 days. Vision is gradually restored, after the epithelium has healed (from the third day) so vision is significantly improved. The contact lens usually stays on for about 3-4 days and is removed by the doctor. After removal, vision improves even more.
In the month the qualitative and quantitative vision with both techniques are similar.
The return to activities takes place from the next day in LASIK and Fempto-Lasik and after three days in PRK & Trans-PRK. Your surgeon will suggest postoperative follow-up.
Are There Complications In Refractive Surgery?
Laser refractive surgery is not an emergency procedure such as a major cataract surgery or advanced glaucoma. It is the choice of the individual (for various reasons) in codecision with the Ophthalmic Surgeon. A significant degree of myopia makes the person unable to see the basic objects in their immediate environment.
The risks from the daily use of contact lenses (severe corneal infections, ulcers, etc.) are four (4) times greater than the Laser, as recorded through validated studies.
No medical invasive procedure completely excludes the side effect. Myopia Lasers can cause side effects such as dry eye, correction, hypercorrection, infection, haze, keratectasia, dry eye, etc., which are usually corrected with appropriate close postoperative monitoring.
What is the cost of the Laser? Is it tolerable?
It is very reasonable, a multiple of the cost that one will need in one’s life for both glasses and contact lenses. Refractive eye surgery that has the ability to undergo laser is a permanent solution, while it is profitable in the long run and economically.
Finally, what is the goal of a refractive surgery and what is its success rate?
The goal of laser surgery is to detoxify from glasses and contact lenses and of course the best possible vision by improving the daily life of the person.
Eye safety should always be a primary concern.
The results are impressive.
Those who have undergone myopia laser surgery say that the laser for detoxification from glasses and lenses was the best gift they have given themselves.
The success of laser myopia now stands at 99% with very modern machines with a deviation of +/- 0.50 for a moderate-significant myopia. The operation is now considered very successful, very reliable and very safe, with the use of all these preoperative control machines. In some rare cases, auxiliary glass for night driving is not excluded. People over the age of 45 may need laser glass after reading due to presbyopia, while before myopia surgery, no auxiliary was needed.
close glass. If one does not want to wear glasses even close, then the technique “Monovision” is done, where the non-dominant eye is corrected, so that a small amount of myopia is left that will help close.
Refractive surgery is one of the safest, most successful and effective surgeries performed on the human body.
The satisfaction for the result is great, depending on the level of expectations of each candidate. The best possible postoperative satisfaction of the person who underwent the laser is related to the excellent cooperation, the correct choice of technique, the “good eye” & the Ophthalmologist.
Medical Center: 2 Thiseos Str., Maroussi
Tel: 210 8055260 & 6945 904252
www.barla.gr [email protected]